The Good Doctor: The One who Preserves Life or Ends Suffering?
- Kavya Reddy
- Sep 7, 2025
- 7 min read
By: Kavya Reddy; Edited By: Krithi Kankanala

In today’s world, we are obsessed with staying young and are in denial of our mortality. From anti-inflammatory diets to anti-ageing skincare, we are constantly told that we must prolong our lives for as long as possible. Alongside this, a fear of death has been instilled in us since childhood. But what about those who seek assisted suicide? What makes them turn against the societal push to live and choose death instead? In this article, we will explore the complex moral, ethical, and economic dilemmas of assisted suicide, and examine how the system works and whether it can be improved.
According to Britannica, assisted suicide “is a procedure in which people take medications to end their own lives with the help of others, usually medical professionals”. Many argue that “assisted suicide” is a harmful term, that it is offensive and inaccurate. It paints a picture of a suicidal patient, rather than a patient who wants to choose a painless death on their own terms. The term “assisted dying” or “medical death” is a more accurate description of what the law permits. This is different from euthanasia, in which a “doctor is allowed by law to end a person’s life by a painless means, as long as the person and their family agree”. The mass legalisation of assisted suicide has been slow, stalled by ethical concerns and public backlash. Only a handful of countries—mainly Western ones such as Australia, Belgium, Canada, and Switzerland—have legalised the procedure.

The process
Assisted suicide has three main steps: Request and assessment, Administration of the substance, and After death. Patients will need to submit oral and written requests, after which physicians will extensively assess whether they meet the eligibility criteria. To be eligible in the United States, you must have a terminal illness, be 18 years or older, be able to make healthcare decisions, and be capable of consuming the medication. If the physicians approve your requests, you will be given a prescription for lethal medication, which often involves a combination of sedative drugs such as barbiturates and morphine sulfate. Patients have the right to withdraw at any point in this process, and should not be coerced by physicians to make a certain decision.
The war on death
From its inception, assisted suicide has been a topic of contention. It has been surrounded by questions about its ethical code, power dynamics and societal impact. This article aims to unpack both sides of the argument, understand the different motivations behind assisted suicide and its potential effects on society and the economy.
Dying with dignity
People with terminal illnesses such as cancer and treatment-resistant mental health issues like depression experience a huge drop in their quality of life. Their days are spent in chronic pain, they suffer from limited mobility, and spend much of their lives in hospital rooms, unable to live on their own terms. Supporters of assisted suicide argue that it allows patients to die with dignity. It provides them with a quick and painless death, as opposed to letting their illness take its course, eroding their dignity and sense of self. It also allows patients to exercise their right to choose and have autonomy over their lives, including how and when they die.
In January of 2018, Aurelia Brouwers chose to end her life with voluntary euthanasia, as she struggled with psychiatric illnesses such as borderline personality disorder, chronic depression and suicidal tendencies. However, many psychiatrists questioned her doctors, as they claimed that it is not possible to know whether she was mentally fit to make that decision on her own, or if it was her suicidal tendencies. "How could I know - how could anybody know - that her death wish was not a sign of her psychiatric disease? The fact that one can rationalise about it does not mean it's not a sign of the disease," says psychiatrist Dr Frank Koerselman, one of the Netherlands' most outspoken critics of euthanasia in cases of mental illness. Brouwers’ case highlights the complex nature of assisted deaths. A doctor can never state with complete certainty whether a patient is in the right frame of mind when they decide to undergo assisted suicide.
Ethical Concerns
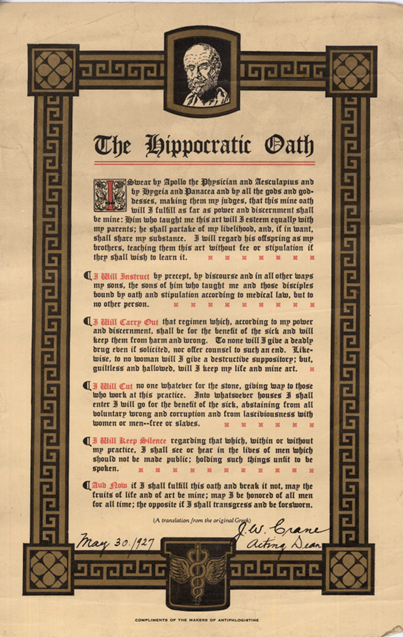
Meanwhile, critics argue that the concept of assisted dying violates the Hippocratic Oath, which states that physicians will keep their patients “from harm and wrong”. A doctor must prolong and preserve life, and by facilitating patients to end their lives, they are doing harm. “Granting patients the right to die gives doctors a ‘duty to kill,’ which violates their professional code. Furthermore, a ‘right to die’ for some people might well become a ‘duty to die’ by others, particularly those who are vulnerable or dependent upon others. It also raises concerns about the power dynamic in this relationship, where doctors may abuse this power and kill patients without their consent. A study conducted in 2012 shows that “32% of the assisted deaths in Belgium are carried out without request and 47% of assisted deaths go unreported in the Flanders region of Belgium”. This is a worrying statistic as it highlights the unregulated nature of this industry and the lack of accountability in the healthcare system. Ultimately, this demonstrates that poor regulatory standards, lack of enforcement and government oversight can turn assisted suicide into mass murder.
In Canada, Roger Foley filed a lawsuit against the government-affiliated Victoria Hospital in Ontario for allegedly encouraging him to opt for assisted death, instead of paying for continued treatment. “They asked if I want an assisted death. I don’t. I was told that I would be charged $1,800 per day [for hospital care]. I have $2 million worth of bills. Nurses here told me that I should end my life”. This paints a worrying picture of how MAID (Medical Assistance In Dying) can be misused, and how vulnerable people could be forced into opting for assisted suicide.
But what happens when people start to choose assisted death, not because of chronic illnesses, but simply because choosing to live is too expensive? It exposes the flaws of Western countries: overstretched healthcare spending, excessive burden on hospitals, and overworked healthcare workers, making it nearly impossible to implement an ethical assisted suicide program.

Human rights experts from the United Nations have expressed concerns that the MAID program will encourage older adults and people living with disabilities to opt for premature death because of unaffordable treatment or living costs. There have been cases in Canada where patients with disabilities paused or cancelled their assisted death requests after receiving accessible housing. In the long run, people may opt for MAID, not because of their desire to die, but simply for a lack of options. It ceases to uphold patient autonomy, as people are making this decision not because of incurable illnesses, but simply because of unfavourable economic circumstances. This is a superficial band-aid on the failings of the healthcare system and does not hold the government accountable for excluding poorer communities from healthcare access.
What does this mean for the economy?
Supporters of assisted suicide argue that it will become an essential part of developed economies in the future. By 2050, the global population aged 60 and over is projected to reach 2.1 billion – more than double its 2020 figure. At the same time, low birth rates and a shrinking younger demographic will also lead to changes in government spending. Rising healthcare expenditure, pension payouts and increasing life expectancy put a massive strain on insufficient national budgets. We can already see this phenomenon in Japan, where a large senior population, coupled with low birth rates, has severely impacted its growth rates. As long-term care becomes unaffordable, patients have to rely on informal care networks. Younger family members often have to shoulder the burden of taking care of ageing relatives, leading to reduced workforce participation and an overall decrease in the productivity of the labour force. The use of advanced technology and AI will reduce healthcare costs, making it more affordable and accessible. However, governments preparing for future population trends might have to consider implementing assisted suicide to ease the pressure on depleting resources.

Economists argue that assisted suicide benefits the economy, with a 2017 research paper predicting that Medical Assistance In Dying (MAID) could save Canada $34.7 million to $138.8 million in health care spending annually. These resources could be allocated to fund the treatment of patients who would have been unable to pay for it otherwise. Assisted suicide also allows patients to donate healthy organs, which could help make organ transplants more accessible and slow the demand for black market organs.
Changes to the system
To preserve the ethos of assisted suicide, we need strict regulations, accessible healthcare, and an ethical healthcare system- a combination that is almost impossible to achieve. In a world dominated by capitalism, where human lives are valued in money, governments cannot be trusted to implement assisted suicide programs with integrity. Maintaining control of this system is also impossible in a healthcare system where staff are overworked, underpaid and burnt out. The conversation around assisted suicide draws attention to the exclusionary policy-making in western countries, and the apathy towards chronically ill, disabled and poor people. For them, the cost of living is a burden, a burden bigger than death.
A possible alternative model for the government-assisted suicide program is for it to be taken up by non-governmental organisations which are not at the mercy of state budgets. Organisations that operate independently and are financed through multiple streams, such as crowdfunding, philanthropists, and government, could help ensure that one party’s interests do not adversely influence the assisted suicide programs. Along with this, there should be stricter screening protocols and mandatory counselling services to properly assess the mental health of patients and understand their motivations for applying. However, this system is not without its flaws. Securing sufficient funding from enthusiastic supporters of assisted suicide might prove to be a challenge. It would also be difficult to create a system that balances both patient autonomy and the opinions of experienced healthcare professionals. But if we do not explore alternative solutions, we risk creating a world in which the power of death is unlawfully sold without consequence. A world in which socioeconomically vulnerable patients are coerced to die in the hands of Grim Reapers disguised as healthcare workers.



Comments